- I’ll explain it in detail
- 1. ** Model construction**
- 2. Clinical verification
- The core’s found
- 1. Patients “look older”
- 2. FaceAge is better than the doctor’s subjective judgment and traditional age
- Why is this research important?
- The value of clinical applications
- The technology’s innovative
- The limits and the challenges
In clinical practice, the doctor usually assesses the patient’s health status or length of life on the basis of his or her face, state and subjective impressions. ** “Language of life”** - that is, the extent to which a person’s physical ageing may reflect health status, therapeutic tolerance and survival expectations more than the actual age (year of birth). However, low-cost standardized biological age assessment tools are lacking. The study developed FaceAge — an in-depth learning system using ** facial photos** to extrapolate “bioage” and to verify whether it can better predict the lifetime of cancer patients than traditional methods. ** Results of the study**
-
AI can accurately estimate “bioage” through facial photographs and independently predict the lifetime of cancer patients.
-
** FaceAge is a better representative of the patient’s state of health than the actual age** and the risk of death rises by about 15 per cent for each “looking old” age of 10 years.
-
** Cancer patients are on average 4.8 years older than their peers “looks older”, ** especially smokers are older in facial organisms.
-
** In terminal cancer palliative treatment, FaceAge improved the accuracy of doctors ‘ projections of six months of survival** AUC was raised from 0.74 to 0.80.
-
FaceAge is significantly associated with genes associated with cellular aging (e.g. CDK6), showing its potential as a biomarker of “molecular aging”.
I’ll explain it in detail
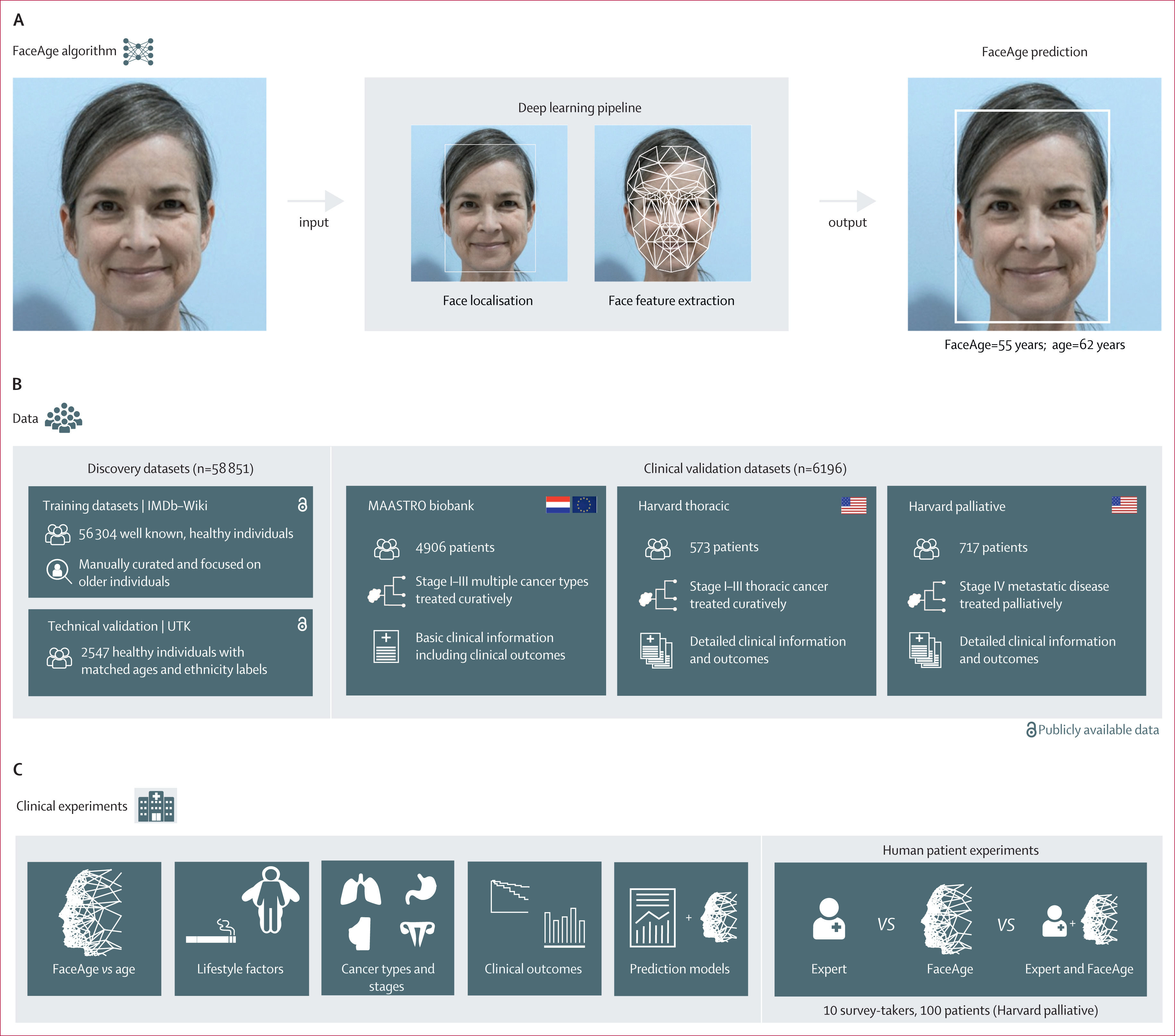
1. ** Model construction**
-
Training and in-depth learning models with over 58,000 photographs using open data sets (IMDb-Wiki and UTKFace);
-
The model structure is based on the Inculation-ResNet v1 network, which begins with human face recognition and then returns to projected age.
2. Clinical verification
The model was validated in three clinical cancer patient data pools:
-
MAASTRO
-
Harvard Thoracic (pulmonary cancer)
-
Harvard Palliative.
The facial photographs were taken from the site of the visit and were semi-standardly taken by medical personnel.
#3 ** Comparison and analysis**
-
Comparison of FaceAge with real age and inclusion in multifactor survival analysis (Cox model);
-
Comparison of the forecast results with the manual judgement of the doctor (including clinical information);
-
Introduction of clinical risk scoring systems such as the TEACHH model to test FaceAge ‘ s ability to enhance its predictive effects;
-
Analyzing whether FaceAge is statistically relevant to genes associated with ageing (e.g. CDK6).
The core’s found
1. Patients “look older”
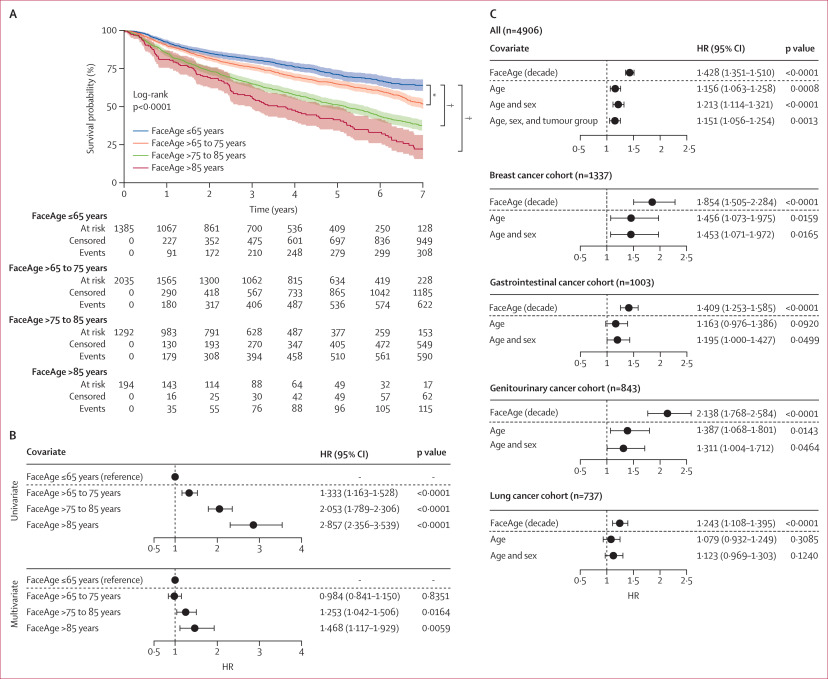
In multiple cancer queues,** the risk of death has increased significantly for each “looks” 10 years old** (HR about 1.15) and is independent of the actual age, sex, and type of tumor.

-
FaceAge is highly associated with the risk of death,** increased by 10 years for each “face biological age” and increased risk of death**: MAASTRO queue: HR 1.151 (p = 0.013)
-
Thoracic queue: HR 1.148 (p = 0.011)
-
Palliative queue: HR 1.117 (p = 0.021)
** FaceAge has an independent predictive power in multiple cancer types (meat, digestive tract, urinary tract, etc.).
2. FaceAge is better than the doctor’s subjective judgment and traditional age
-
When predicting the six-month survival of cancer patients, FaceAge models are superior to doctor’s vision;
-
In integrating clinical models (e.g. TEACHH),** replacing age with FaceAge with model performance (AUC up to 0.80)**;
-
FaceAge effects have remained stable in different cancer types, therapeutic intent (emission vs) and in the course of the disease.
Cox Multi-factor regression analysis:
-
After controlling variables such as sex, cancer, therapeutic intent, phasing, PS rating, etc.: ** FaceAge still predicts a significant lifetime, while the actual age is no longer significant** (Thoracic queue: FaceAge p=0.011, age p=0.16).
-
The inclusion of FaceAge in the model has resulted in a significant increase in model interpretation (log-likehood has increased significantly).
Substitution of the “age” variable in the TEACHH survival rating model:
-
Risk scoring system ** Distinguishing between different life zones after replacing traditional age with FaceAge**: The median survival of high-risk groups decreased (more precise): 0.21 vs 0.24 years;
-
C-index (forecast consistency) has also increased.
#3. FaceAge can assist doctors to make more accurate terminal predictions Experimental design:
-
100 photographs of terminal cancer patients for survival prediction missions (whether or not they have survived for more than six months): Participants included oncologists, inpatients, non-clinical researchers;
-
Provision of: photos only, photographs + medical records, photographs + medical records + FaceAge model outputs.
Results:
-
AUC is about 0.61 when the doctor only looks at the photograph;
-
Upgraded to 0.74 with medical records;
-
Added to the FaceAge projection further up to 0.80 (p<0.0001);
-
** The accuracy of the doctor ‘ s predictions has improved significantly, especially for those with less basic judgement**
4. FaceAge is related to the aging-related molecular mechanisms
-
FaceAge is significantly associated with cellular aging regulation of genes CDK6;
-
The actual age is not statistically relevant to these genes**;
-
Description: FaceAge not only captures visual information, but is more likely to reflect deep biological ageing mechanisms.
#5. ** The “face biological age” of cancer patients is about 4.8 years higher than that of ordinary people**
-
FaceAge for cancer patients was found to be significantly older than their actual age compared to the healthy population (4.79 years more on average, p. < 0.0001);
-
A consistent trend has been observed in the sub-groups of cancer, smoking status, BMI, ECOG performance rating, etc.;
-
Current smokers FaceAge are about more than never smokers ** 33 months**, indicating that models are sensitive to lifestyle variables.
Why is this research important?
The value of clinical applications
-
Quick, low-cost, non-intrusive: only one photo of the face is required;
-
Be suitable for such key options as “therapeutic treatment” and “how to treat” that are common in the clinical context;
-
Providing more precise and objective assessments of survival and reducing errors resulting from subjective judgements;
-
Possibilities to be used in Clinical trial population stratification and to improve the quality of research.
The technology’s innovative
-
For the first time, a systematic study was carried out on “mass biological age” as a medical predictor**;
-
Models are validated from real, heterogeneous, multi-centric clinical queues;
-
Interdisciplinary integration with AI technology and molecular biology.
The limits and the challenges
-
** Training data are not fully healthy or standardized** and there may be deviations (e.g. too many photographs of public figures);
-
** The capacity for trans-racial profiling** was not validated, although the model was initially tested in the multi-ethnic database;
-
Ethical and privacy risks: facial data are extremely sensitive and should be carefully managed and regulated in the future;
-
** Not yet used in clinical practice**, requiring a larger number of central validations and regulatory clearances.
Papers: https://www.thelancet.com/journals/landig/article/PIIS2589-7500(25)00042-1/fulltext